Triple Sugar Iron Agar (TSI): Principle, Procedure and Interpretation
Whenever you see the name of this test i.e. Triple Sugar Iron Agar ,you have to remember that it’s a test which has three sugar (Lactose, Sucrose, and Glucose) and also iron; and it contains Agar Agar as solidifying agent (TSI is a semi solid media having slant and butt).
CLUE: You might have (or not) realized the rationale behind the use of three different sugar and adding iron. Lets start with very basic information and we will proceed towards principle and interpretations.
Composition of Triple Sugar Iron Agar (TSI)
Lactose, Sucrose and Glucose in the concentration of 10:10:1 (i.e. 10 part Lactose (1%), 10 part Sucrose (1%) and 1 part Glucose (0.1%)). TSI is similar to Kligler’s iron agar (KIA), except that Kligler’s iron agar contains only two carbohydrates: glucose (0.1%) and lactose (1%).
Lactose, Sucrose and Glucose in the concentration of 10:10:1 (i.e. 10 part Lactose (1%), 10 part Sucrose (1%) and 1 part Glucose (0.1%)). TSI is similar to Kligler’s iron agar (KIA), except that Kligler’s iron agar contains only two carbohydrates: glucose (0.1%) and lactose (1%).
- 0.1% Glucose: If only glucose is fermented, only enough acid is produced to turn the butt yellow. The slant will remain red
- 1.0 % lactose/1.0% sucrose: a large amount of acid turns both butt and slant yellow, thus indicating the ability of the culture to ferment either lactose or sucrose.
- Iron: Ferrous sulfate: Indicator of H2S formation
- Phenol red: Indicator of acidification (It is yellow in acidic condition and red under alkaline conditions).
- It also contains Peptone which acts as source of nitrogen. (Remember that when ever peptone is utilized under aerobic condition ammonia is produced)
Procedure for Triple Sugar Iron Agar (TSI) Test
- With a sterilized straight inoculation needle touch the top of a well-isolated colony
- Inoculate TSI Agar by first stabbing through the center of the medium to the bottom of the tube and then streaking on the surface of the agar slant.
- Leave the cap on loosely and incubate the tube at 35°C in ambient air for 18 to 24 hours.
Why Sucorse is added in TSI?
Addition of sucrose in TSI Agar permits earlier detection of coliform bacteria that ferment sucrose more rapidly than lactose. Adding sucrose also aids the identification of certain gram-negative bacteria that could ferment sucrose but not lactose. Other basic understanding is TSI Tube contains butt (poorly oxygenated area on the bottom) slant (angled well oxygenated area on the top).
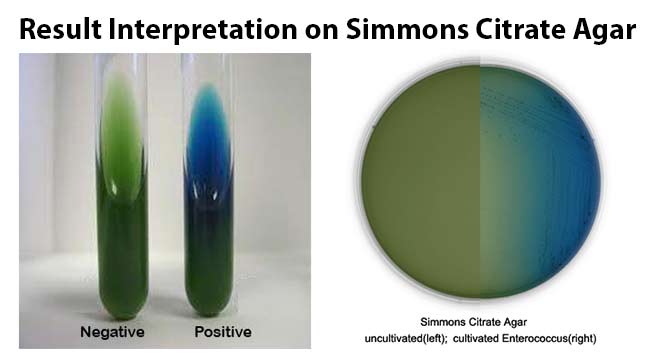
Interpretation of Triple Sugar Iron Agar Test

- If lactose (or sucrose) is fermented, a large amount of acid is produced, which turns the phenol red indicator yellow both in butt and in the slant. Some organisms generate gases, which produces bubbles/cracks on the medium.
- If lactose is not fermented but the small amount of glucose is, the oxygen deficientbutt will be yellow (remember that butt comparatively have more glucose compared to slant i.e. more media more glucose), but on the slant the acid (less acid as media in slant is very less) will be oxidized to carbondioxide and water by the organism and the slant will be red (alkaline or neutral pH).
- If neither lactose/sucrose nor glucose is fermented, both the butt and the slant will be red. The slant can become a deeper red-purple (more alkaline) as a result of production of ammonia from the oxidative deamination of amino acids (remember peoptone is a major constitutents of TSI Agar) .
- if H2S is produced, the black color of ferrous sulfide is seen.
So the expected results of TSI Agar test are:

Image source: Clark College
- Alkaline slant/no change in butt (K/NC) i.e Red/Red = glucose, lactose and sucrose non-fermenter
- Alkaline slant/Alkaline butt (K/K) i.e Red/Red = glucose, lactose and sucrose non-fermenter
- Alkaline slant/acidic butt (K/A); Red/Yellow = glucose fermentation only, gas (+ or -), H2s (+ or -)
- Acidic slant/acidic butt (A/A); Yellow/Yellow = glucose, lactose and/or sucrose fermenter gas (+ or -), H2s (+ or -).
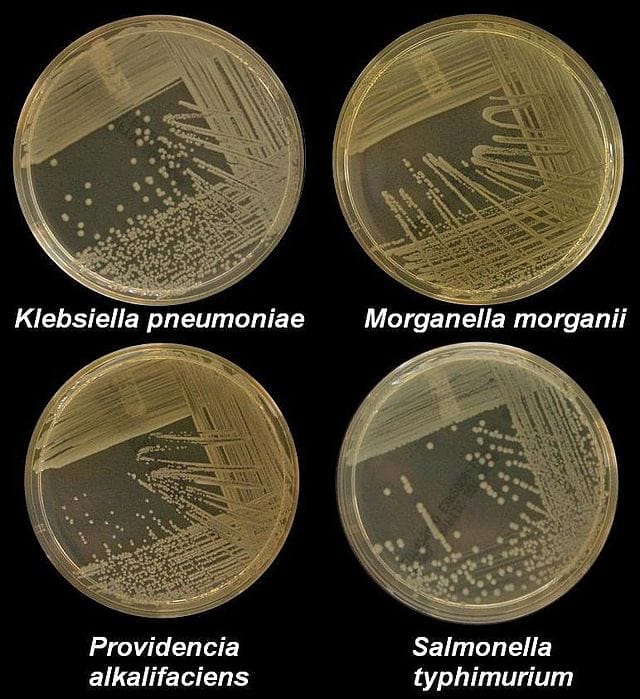
Some example of Triple Sugar Iron (TSI) Agar Reactions:
| Name of the organisms | Slant | Butt | Gas | H2S |
| Escherichia, Klebsiella, Enterobacter | Acid (A) | Acid (A) | Pos (+) | Neg (-) |
| Shigella, Serratia | Alkaline (K) | Acid (A) | Neg (-) | Neg (- ) |
| Salmonella, Proteus | Alkaline (K) | Acid (A) | Pos (+) | Pos (+) |
| Pseudomonas | Alkaline (K) | Alkaline (K) | Neg (-) | Neg (-) |